Abstract
Background: Primary CNS lymphoma (PCNSL) is a rare and highly aggressive variant of non-Hodgkin lymphoma that involves the brain, leptomeninges, spinal cord, or eyes. Among several prognostic models for PCNSL, the International Extranodal Lymphoma Study Group (IELSG) prognostic score is one of the most widely used prognostic models. It is based on age, Eastern Cooperative Oncology Group (ECOG) Performance status (PS), serum lactate dehydrogenase (LDH) level, cerebrospinal fluid (CSF) total protein concentration, and involved regions of the brain. However, IELSG prognostic score can't be evaluated in all patients, because CSF analysis can't be performed in patients with high risk of brain herniation or difficulty in cooperation. β2-microglobulin is a small protein in the essential part of major histocompatibility complex class I molecules, and elevated serum β2-microglobulin levels were found to be associated with poor prognosis in various types of lymphoma. Nevertheless, the prognostic value of serum β2-microglobulin in PCNSL patients has not yet been specifically investigated. In this study, we aimed to evaluate the prognostic value of serum β2-microglobulin and to propose a risk-stratifying classification according to serum β2-microglobulin levels for patients with PCNSL.
Methods: Between October 2002 and August 2019, 298 patients were newly diagnosed with PCNSL at Asan Medical Center, Seoul, South Korea. After excluding patients with no baseline serum β2-microglobulin level, 282 patients were included in this retrospective analysis. Primary end point was overall survival (OS). OS was defined as the time interval from the date of initial diagnosis to the date of death from any cause. Serum β2-microglobulin was measured using a radioimmunoassay kit and the upper normal limit (UNL) of serum β2-microglobulin was 2.4 mg/L. Key baseline characteristics and candidate prognostic factors including age, sex, ECOG PS, serum β2-microglobulin level, serum LDH level, CSF total protein concentration, and involved regions of the brain were included in the univariate analysis. In the multivariate analysis, variables which showed significant association with OS (p < 0.05) in the univariate analyses were included.
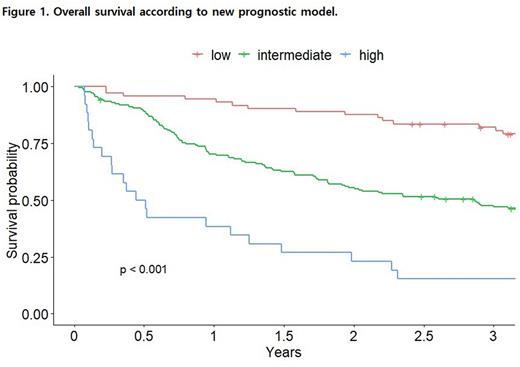
Results: The median age was 59.9 years (range, 17-86), 150 patients (53.2%) were male, 78 patients (27.7%) had ECOG PS > 1, and 98 patients (34.8%) had an elevated serum LDH level (> UNL). Two-hundred-seventy-seven patients (98.2%) received HD-MTX-containing chemotherapy as first-line-treatment. With a median follow-up duration of 3.0 years (range, 0.03-16.4), the median OS was 3.7 years (95% confidence interval [CI], 2.9-4.7). In the univariate analysis, age of > 60 years, ECOG PS > 1, high serum LDH serum level (> UNL), and high serum β2-microglobulin level (> 2.4 mg/L) showed significant association with poor OS (p < 0.05). In the multivariate analysis, high serum β2-microglobulin level (hazard ratio [HR], 1.69; 95% CI 1.07-2.68; p = 0.025), age of > 60 years (HR, 1.67; 95% CI 1.22-2.28; p = 0.001), ECOG PS > 1 (HR, 1.99; 95% CI, 1.44-2.75; p < 0.001) and high serum LDH level (HR, 1.46, 95% CI 1.07-1.99; p = 0.016) were all independently associated with poor OS. We developed a new prognostic model based on these risk factors, in which patients were stratified into three groups according to the total number of risk factors: low (no risk factor), intermediate (1 or 2 risk factors) and high (3 or 4 risk factors). Median OS was 7.1, 2.9, and 0.5 years (p < 0.001) in low- (N = 73, 25.9%), intermediate- (N = 183, 64.9%), and high-risk groups (N = 26, 9.2%), respectively (Figure 1). As this prognostic model was developed in a single center, we tried to validate this model in an independent validation cohort from two other large medical centers in South Korea. However, validation could not be performed due to too many missing β2-microglobulin values.
Conclusions: Serum β2-microglobulin level is an independent prognostic factor in newly diagnosed patient with PCNSL. The proposed β2-microglobulin-based prognostic model, which is based on easily obtainable clinical and laboratory data, might be simple and useful tool to predict prognosis in these patients. This prognostic model deserves further validation in an independent cohort.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal